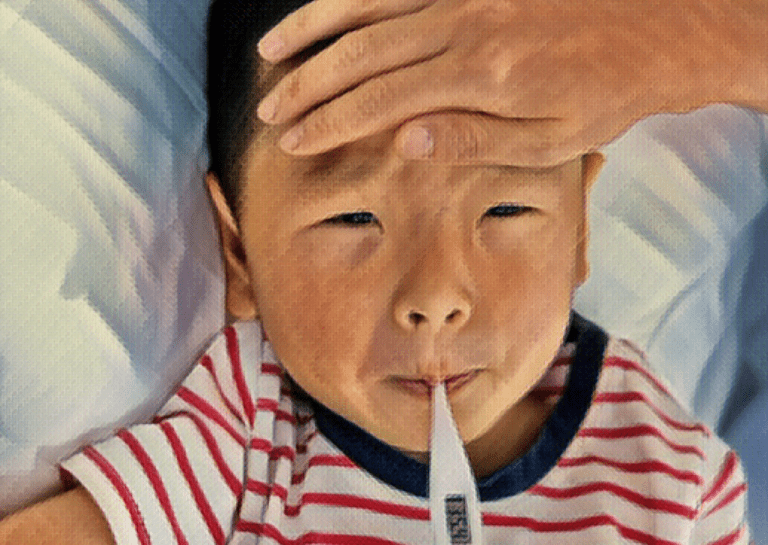
Meningitis is the infection of the meninges; the tissues surrounding the brain and spinal cord. There are 2 types of meningitis — bacterial and viral meningitis. Meningitis is characterized by fever, headache, and neck stiffness, and is often caused by infections in other parts of the body that travel through the bloodstream to the meninges.
This article covers the different types of meningitis as well as the signs and symptoms that parents should be aware of, including the diagnosis and treatment of both viral and bacterial meningitis.
Table of contents
Types of Meningitis
Viral meningitis
Viral meningitis is caused by viruses. It is the most common of the two types but is generally less dangerous than bacterial meningitis. Enteroviruses are most often responsible for causing viral meningitis and are similar to common cold viruses spread through coughing and sneezing. These types of viruses often cause only mild illness but can be serious if they cause a Central Nervous System (CNS) infection such as meningitis.
Common features
The features of viral meningitis are typically similar to those of bacterial meningitis, but less severe.
- Infants: In infants, viral meningitis is characterized by abrupt fever, irritability, lethargy, poor feeding, rash, vomiting, diarrhea, neck stiffness (less common in infants than older children), bulging fontanel (soft spot on a baby’s head), as well as seizures in the absence of fever. Other manifestations include pneumonia, inflammation of the liver, and inflammation of the heart tissue.
- Children and adolescents: Common features of viral meningitis include fever, headaches, nausea, neck stiffness, vomiting, rash, and photophobia (light sensitivity).
Bacterial meningitis
Bacterial meningitis is most commonly seen in infants younger than 2. It occurs when bacteria enter the bloodstream, usually through a preexisting infection of the sinuses or the mastoid bone behind the ear. Bacterial infections can also occur through trauma, neurosurgery, Cerebrospinal Fluid (CSF) leaks from a head injury, or through medical devices such as CSF shunts or cochlear implants.
Common features
- Infants: Bacterial meningitis in infants often manifests as fever or hypothermia, lethargy, irritability, poor feeding, bulging fontanel, vomiting, diarrhea, breathing problems, jaundice, and seizures.
- Children and adolescents: Common features of bacterial meningitis in children and adolescents include fever, headaches, neck stiffness, light sensitivity, nausea, vomiting, confusion, irritability, and lethargy.
Diagnosis
Prompt diagnosis and treatment of meningitis is crucial as untreated meningitis can be fatal. It is also important to distinguish between bacterial and viral meningitis. When a child is taken to a hospital with suspected meningitis, they are usually assumed to have bacterial meningitis until it is ruled out. This is because bacterial meningitis is a medical emergency and must be treated as soon as possible or until a firm diagnosis for viral meningitis is reached.
Diagnosis for meningitis typically involves:
- Obtaining a history of the child’s symptoms, any predisposing factors (e.g. immunodeficiency), their immunization history, and any drug allergies.
- Performing a physical examination to check vital signs and to identify physiological signs associated with meningitis.
- Assessing the child’s mental status and level of consciousness.
- Taking blood samples for testing.
- Performing a lumbar puncture (‘spinal tap’) to extract CSF for diagnostic testing.
The main diagnostic indicator for meningitis is CSF. Doctors will examine samples taken from lumbar punctures to check for abnormalities and to rule out other conditions that present similar signs to meningitis.
Both types of meningitis appear very similar and it can be a diagnostic challenge to distinguish between the two. Viral meningitis is ultimately diagnosed by examining CSF for viral pathogens and proving that there are no bacterial cultures present.
Treatment
Treatment for meningitis involves managing the symptoms and effects of the illness and treating the underlying cause, be it bacterial or viral.
Bacterial meningitis
Bacterial meningitis is treated through wide-spectrum empiric antibiotic therapy. This is combined with supportive care measures to manage the effects of the illness where needed, such as managing cardiovascular instability or shock, providing oxygen and respiratory support, fluid therapy, hypoglycemia (low blood sugar) prevention, seizure control, and nutritional support.
Viral meningitis
Most cases of viral meningitis are treated symptomatically, and empiric antibiotic therapy is generally used when there is a risk of bacterial meningitis. Supportive care measures for viral meningitis involve letting the child rest in a quiet, dimly lit room, treating headache, fever, and pain with acetaminophen or ibuprofen, and fluid therapy if the child’s oral intake is poor.
Prevention
There are preventative measures parents and caregivers can take to protect themselves and their children from meningitis.
- Hygiene: Hygienic measures such as handwashing after diaper changes can help prevent the spread of enteroviruses.
- Vaccines: Having your child vaccinated against specific viruses helps protect them from viral meningitis.
Personal protection: Taking measures to protect against insect bites and tick exposure (e.g. insect repellant) reduces the risk of contracting viruses.
References
- Rotbart HA. Viral meningitis. Semin Neurol. 2000;20(3):277-92. doi: 10.1055/s-2000-9427. PMID: 11051293.
- Britton PN, Dale RC, Nissen MD, Crawford N, Elliott E, Macartney K, Khandaker G, Booy R, Jones CA; PAEDS-ACE Investigators. Parechovirus Encephalitis and Neurodevelopmental Outcomes. Pediatrics. 2016 Feb;137(2):e20152848. doi: 10.1542/peds.2015-2848. Epub 2016 Jan 20. PMID: 26791970.
- Romero JR, Newland JG. Viral meningitis and encephalitis: traditional and emerging viral agents. Semin Pediatr Infect Dis. 2003 Apr;14(2):72-82. doi: 10.1053/spid.2003.127223. PMID: 12881794.
- Thigpen MC, Whitney CG, Messonnier NE, Zell ER, Lynfield R, Hadler JL, Harrison LH, Farley MM, Reingold A, Bennett NM, Craig AS, Schaffner W, Thomas A, Lewis MM, Scallan E, Schuchat A; Emerging Infections Programs Network. Bacterial meningitis in the United States, 1998-2007. N Engl J Med. 2011 May 26;364(21):2016-25. doi: 10.1056/NEJMoa1005384. PMID: 21612470.
- Overall JC Jr. Neonatal bacterial meningitis. Analysis of predisposing factors and outcome compared with matched control subjects. J Pediatr. 1970 Apr;76(4):499-511. doi: 10.1016/s0022-3476(70)80399-7. PMID: 5420788.
- Ouchenir L, Renaud C, Khan S, Bitnun A, Boisvert AA, McDonald J, Bowes J, Brophy J, Barton M, Ting J, Roberts A, Hawkes M, Robinson JL. The Epidemiology, Management, and Outcomes of Bacterial Meningitis in Infants. Pediatrics. 2017 Jul;140(1):e20170476. doi: 10.1542/peds.2017-0476. Epub 2017 Jun 9. PMID: 28600447.
- Kim KS. Bacterial meningitis beyond the neonatal period. In: Feigin and Cherry’s Textbook of Pediatric Infectious Diseases, 8th, Cherry JD, Harrison GJ, Kaplan SL, et al (Eds), Elsevier, Philadelphia 2019. p.309.
- Mintegi S, García S, Martín MJ, Durán I, Arana-Arri E, Fernandez CL, Benito J, Hernández-Bou S; Meningitis Group of the Spanish Society of Pediatric Emergencies. Clinical Prediction Rule for Distinguishing Bacterial From Aseptic Meningitis. Pediatrics. 2020 Sep;146(3):e20201126. doi: 10.1542/peds.2020-1126. Epub 2020 Aug 25. PMID: 32843440.
- Tunkel AR, Hartman BJ, Kaplan SL, Kaufman BA, Roos KL, Scheld WM, Whitley RJ. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2004 Nov 1;39(9):1267-84. doi: 10.1086/425368. Epub 2004 Oct 6. PMID: 15494903.