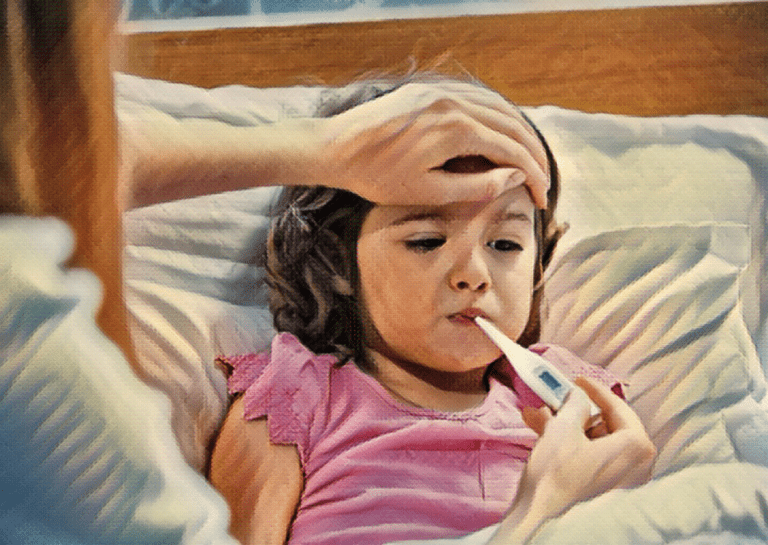
A fever is one of the most common afflictions seen in babies and young children and is indicated by an increase in body temperature above the normal range (97.9˚F-99˚F). Any temperature above 100.4˚F constitutes a fever and can suggest infection or illness.
Fevers in babies and children can be a cause for concern for any parent, but understanding the associated symptoms and knowing when to see a doctor will help you navigate this common problem.
Symptoms
When your child has a fever, their elevated body temperature will often be accompanied by additional symptoms. These can take 24 hours to develop. The type and severity of the accompanying symptoms can indicate the underlying cause of the fever. It’s important to be able to identify these symptoms so you can accurately explain your child’s condition to a doctor over the phone.
Common symptoms include:
- Irritability
- Discomfort
- Loss of appetite
- Poor sleeping
- Lethargy
- Rash
- Coughing/sneezing
- Febrile seizures
Causes
What causes fever in babies and children? Fevers most often develop as a symptom of infection. This is because the increase in temperature helps to fight off bacteria and viruses by stimulating the body’s immune system response.
If your child’s temperature exceeds 100.4˚F, it means that they have likely picked up a cold or flu virus and may need medical attention.
A common misconception is that teething causes fever in babies, but this is not necessarily true. Although teething can cause an increase in temperature and discomfort, it is usually only a slight elevation. A temperature above 100.4˚F indicates a different problem.
In general, a temperature of 100-102˚F indicates a low-level fever and does not always require treatment. Your child has an ‘average’ fever if the temperature is between 102 and 104˚F. An average fever does not require treatment unless it is causing your child excessive discomfort.
If a fever exceeds 104 ˚F, you should always treat the fever and seek immediate medical advice.
Common causes of fever include:
- Reaction to vaccination (can last up to 48 hours after immunization)
- Cold/flu
- Ear infections
- UTIs
- Viral respiratory infection
- Gastrointestinal infection
When to call the doctor
Although a fever does not always indicate something serious, there are some situations in which you should seek medical attention for your child.
For Children under 3 months
- Seek medical advice if their rectal temperature exceeds 100.4˚F.
For Children aged 3-6 months
- Seek medical advice if their rectal temperature exceeds 102˚F with accompanying irritability or lethargy.
For Children aged 6-24 months
- Seek medical advice if their temperature is higher than 102˚F with accompanying rash, cough, or persistent diarrhea.
For Children older than 2
- Seek medical advice if your child has a fever accompanied by a rash, headache, lethargy, irritability, neck stiffness, vomiting, or diarrhea.
- Seek immediate medical care if your child has a febrile seizure that lasts longer than 5 minutes, or if their fever does not subside with an appropriate dose of medication.
Tips for taking a child’s temperature accurately
Being able to accurately record and read a child’s temperature is something that is often overlooked. It may seem straightforward, but it’s important to know how to do it correctly as the procedure differs depending on a child’s age. You may also decide on a particular method based on how cooperative your child is or what is most convenient based on their condition.
- For children under 2 years of age, oral thermometers can be inaccurate. Rectal thermometers should be used instead.
- Until 6 months of age, ear temperatures are also an inaccurate measurement of body temperature.
- For children older than 2, a digital thermometer is the most accurate device for temperature readings.
- For taking temperature orally, ensure that you wait 30 minutes after your child has had anything to eat or drink for the most accurate reading.
- Oral thermometers are recommended for children over the age of 4 who are generally more cooperative.
- Note the thermometer readings as well as the date and time you took each reading. This information will be helpful for a doctor or nurse if you seek medical advice
Treatment
It is important to note that babies under 3 months with a fever should be seen by a doctor as soon as possible. But for older babies and children displaying a low-grade or average fever, there are ways to treat them at home. As long as your child is showing no concerning symptoms, their temperature doesn’t exceed 104˚F, and their fever lasts no longer than 72 hours, you don’t need to bring them to the doctor.
Medication such as Acetaminophen can be used for children over 3-months. The appropriate dose depends on the child’s weight, so you may need to weigh your child if you’re unsure. You should always consult a medical professional for advice about medication and dosage.
Additionally, you can cool your child down with lighter clothing or blankets, by keeping their room air-conditioned, and by giving them plenty of fluids to keep them hydrated.
References
Consolini, D. M. et al. “Fever in Infants and Children – Pediatrics”, MSD Manual Professional Edition, MSD Manuals, Last modified June 2020, www.msdmanuals.com/professional/pediatrics/symptoms-in-infants-and-children/fever-in-infants-and-children.
Kliegman, R. M. et al. “Fever”, In Nelson Textbook of Pediatrics. 20th ed. Philadelphia, Pa.: Elsevier; 2016. https://www.clinicalkey.com.
Marx, J. A. et al., eds. “Pediatric fever”, In Rosen’s Emergency Medicine: Concepts and Clinical Practice. 8th ed. Philadelphia, Pa.: Saunders Elsevier; 2014.
Murren-Boezem, J. “How to Take Your Child’s Temperature (for Parents) – Nemours KidsHealth.”, The Nemours Foundation: 2018, kidshealth.org/en/parents/take-temperature.html.
Porter, Robert S, and Fred G Wenger. “Diagnosis and Treatment of Pediatric Fever by Caretakers.” The Journal of Emergency Medicine, vol. 19, no. 1, 2000, pp. 1–4., doi:10.1016/s0736-4679(00)00173-6.