An unconscious child will appear to be asleep and will show no awareness of their environment. They will not respond to attempts to wake them and their awareness will be completely diminished. There are different states of impaired consciousness, ranging from less profound states like lethargy or stupor to more serious conditions such as coma.
A child may fall unconscious for a number of reasons, such as infection, illness, poison exposure, head trauma, metabolic disorders, and seizures.
This article discusses in more detail the different states of impaired consciousness, their possible causes, and the diagnosis and treatment of such conditions.
Table of contents
States of impaired consciousness
The various states of impaired consciousness fall on a spectrum. This spectrum ranges from full arousal (the normal state of being conscious, alert, and aware of your surroundings) to complete unresponsiveness (i.e. coma).
Some of the different states of consciousness on this spectrum are:
Lethargy: Also known as obtundation or stupor, lethargy is a state in which arousal is somewhat impaired and is akin to feeling extremely tired after a lack of sleep. This can manifest as being unable to maintain one’s attention, responding poorly to questions or commands, and falling asleep if not stimulated.
Delirium: Delirium is a state of disturbed consciousness and can be either hyperactive or hypoactive in nature. The former can manifest as hyperactivity and poor sleep, while the latter can result in diminished interaction with surroundings and drowsiness. Someone experiencing delirium may be confused, excited, or irritable, and may also experience hallucinations.
Coma: Coma is described as a transient state of unconsciousness that lasts no longer than 2 to 4 weeks. If a comatose child does not recover or die from their coma, they will either evolve into a state of minimal consciousness or end up in a persistent vegetative state [3]. The latter of these states is the most serious, as it is considered to be a permanent condition with little chance of improvement.
Reasons a child may be unconscious
Causes of coma can be either traumatic or non-traumatic.
Non-traumatic causes: Non-traumatic causes of coma are more common in infancy and early childhood. Among these causes, infection is the most common and makes up 30 to 60 percent of cases.
- Infection (e.g. sepsis, meningitis)
- Toxic exposure/drug overdose
- Metabolic disorders (e.g. hypoglycemia, diabetic ketoacidosis)
- Seizures
- Drowning
- Intracranial hemorrhage/tumor
- Cardiac arrhythmia
- Foreign body aspiration
Traumatic causes:
- Head trauma
- Traumatic brain injury
The prognosis for a child suffering from impaired consciousness usually depends on the underlying cause of their condition. For example, the mortality rate for intoxication is as low as 3.4 percent but rises to 84 percent for drowning [4].
Diagnosis and management
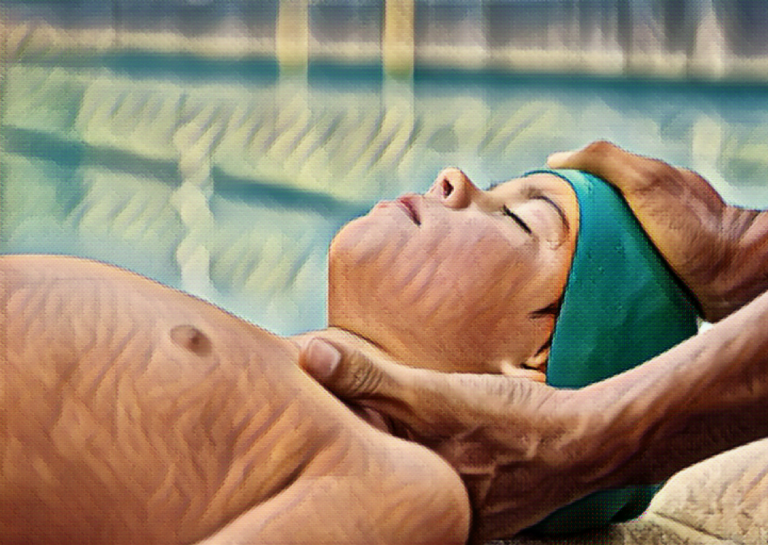
Coma is a medical emergency that must be managed and treated rapidly. A child who is found to be unconscious should receive immediate medical attention. Identifying and diagnosing the underlying cause is crucial to appropriately treat the condition and improve the patient’s prognosis.
The patient’s history is a key part of understanding the underlying cause. For example, an ongoing illness or a known medical condition/injury will more readily indicate the reason for impaired consciousness than something more abrupt and unexpected [6].
Doctors will carry out a physical examination for signs associated with certain causes of coma. Symptoms observed in coma patients can include:
- Tachypnea (abnormally rapid breathing)
- Tachycardia (abnormally rapid heart rate)
- Hypotension (abnormally low blood pressure)
- Abnormal complexion (bruising, pronounced redness, jaundice, purpuric rashes, etc.)
Treatment
Initial treatment for coma involves stabilizing the patient and taking measures to prevent brain injury.
Treatment can involve securing the airway, providing oxygen, administering fluids to treat hypotension, managing seizures, normalizing temperature, and treating/preventing infection.
Neurologic examinations are a key part of understanding and treating coma. Computed Tomography (CT), Magnetic Resonance Imaging (MRI), and Electroencephalogram (EEG) are all important tools for identifying complications of coma and determining the prognosis depending on the underlying cause of the child’s impaired consciousness.
References
- Plum F, Posner JB. The Diagnosis of Stupor and Coma, 3rd ed, Davis FA (Ed), Oxford University Press, Philadelphia 1980. p.2.
- Ashwal S. Medical aspects of the minimally conscious state in children. Brain Dev. 2003 Dec;25(8):535-45. doi: 10.1016/s0387-7604(03)00095-0. PMID: 14580666.
- Multi-Society Task Force on PVS. Medical aspects of the persistent vegetative state (1). N Engl J Med. 1994 May 26;330(21):1499-508. doi: 10.1056/NEJM199405263302107. PMID: 7818633.
- Wong CP, Forsyth RJ, Kelly TP, Eyre JA. Incidence, aetiology, and outcome of non-traumatic coma: a population based study. Arch Dis Child. 2001 Mar;84(3):193-9. doi: 10.1136/adc.84.3.193. PMID: 11207161; PMCID: PMC1718674.
- Bansal A, Singhi SC, Singhi PD, Khandelwal N, Ramesh S. Non-traumatic coma. Indian J Pediatr. 2005 Jun;72(6):467-73. doi: 10.1007/BF02724422. PMID: 15985734.
- Bates D. The management of medical coma. J Neurol Neurosurg Psychiatry. 1993 Jun;56(6):589-98. doi: 10.1136/jnnp.56.6.589. PMID: 8509770; PMCID: PMC489606.
- Coates BM, Vavilala MS, Mack CD, Muangman S, Suz P, Sharar SR, Bulger E, Lam AM. Influence of definition and location of hypotension on outcome following severe pediatric traumatic brain injury. Crit Care Med. 2005 Nov;33(11):2645-50. doi: 10.1097/01.ccm.0000186417.19199.9b. PMID: 16276192; PMCID: PMC1361352.