Zika Virus is a virus transmitted by insects such as mosquitoes and is in the same virus family as Yellow Fever Virus and West Nile Virus. Zika Virus is usually transmitted by the bite of infected mosquitoes. The symptoms and presentation of Zika are nonspecific and can be misdiagnosed as other infectious diseases, especially those spread by arthropods.
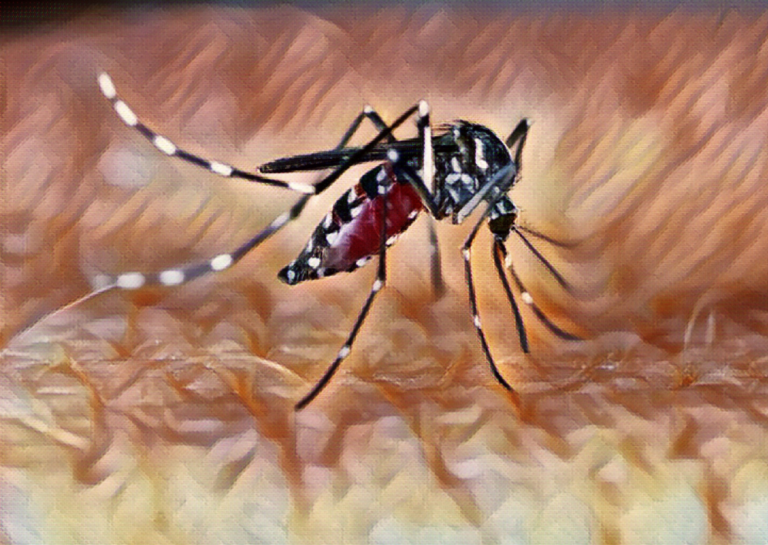
Outbreaks of Zika virus infection have occurred in Africa, Southeast Asia, the Pacific Islands, the Americas, and the Caribbean. In 2015 and 2016, a Zika virus outbreak occurred in the Americas, the Caribbean, and the Pacific. Zika virus is transmitted to humans via the bite of an infected Aedes mosquito.
Table of contents
Symptoms & Types
Transmission
Zika virus may be transmitted to humans via the following:
- Bite of an infected mosquito
- Maternal-fetal transmission
- Sex (including vaginal, anal, and oral sex)
- Blood product transfusion
- Organ transplantation
- Laboratory exposure
Zika virus RNA has been detected in blood, urine, semen, saliva, female genital tract secretions, cerebrospinal fluid, amniotic fluid, and breast milk.
Symptoms in Adults
Symptoms of Zika virus infection occur in 20-25% of individuals who become infected with Zika virus. A symptomatic infection has been described more frequently among women and patients less than 40 years in one study, however, neither female sex nor age was associated with an increased prevalence of infection.
Symptoms include:
- Low-grade fever
- Itchy rash present on the face, trunk, extremities, palms, and soles
- Joint pain, often in the small joints of the hands and feet
- Conjunctivitis (pink eye)
- Muscle pain
- Headache
- Lack of energy
Less commonly observed symptoms and signs include abdominal pain, nausea, diarrhea, and mucous membrane ulcerations.
Clinical diagnosis can be decided if 2 or more of these symptoms are present.
Symptoms in Children
The range of Zika virus infections in children includes intrauterine infection (vertical transmission during pregnancy), intrapartum infection (vertical transmission at the time of delivery), and postnatal infection (transmission via mosquito bites). Symptoms of the Zika Virus in children and similar to those seen in adults, but maybe less prominent.
Zika Virus and Pregnancy
The diagnostic approach is different in pregnant compared with nonpregnant individuals because Zika Virus persists approximately three times longer in a pregnant woman’s serum. The offspring is at risk of major central nervous system anomalies with congenital infection, even if the mother is asymptomatic.
Screening: At the initial prenatal visit, it is reasonable for health care providers to verbally screen pregnant women for possible exposure to Zika before and during the current pregnancy. If travel-associated exposure occurred or the patient lives in an endemic region, providers should also ask about possible symptoms of Zika infection. During an epidemic, screening is performed at each prenatal visit.
Frequency of fetal transmission: The frequency of maternal-to-fetal transmission of Zika is difficult to determine accurately because virus-specific IgM and polymerase chain reaction (PCR) is not positive in all congenitally infected newborns. However, it is clear that the risk for vertical transmission exists throughout pregnancy and in the offspring of both symptomatic and asymptomatic mothers. In a cohort study of 130 infants whose mothers had PCR-confirmed symptomatic Zika in pregnancy, the vertical transmission rate was 65 percent.
Birth defects: Birth defects clearly result from the vertical transmission and in addition, other potential consequences of vertical transmission include fetal loss (miscarriage, stillbirth), hydrops fetalis, fetal growth restriction, neurologic and positional abnormalities, and impaired neurodevelopment. The greatest risk of serious fetal/newborn sequelae appears to be with first- or second-trimester Zika infection, but serious fetal/newborn sequelae also occur with a third-trimester infection.
Diagnosis & Tests
Symptomatic individuals: Zika virus infection is diagnosed through testing serum, urine, or whole blood or via Zika virus serology.
Asymptomatic individuals: There is no role for Zika virus testing in asymptomatic individuals who are not pregnant.
Treatment & Care
There is no specific treatment for Zika virus infection. Management consists of rest and symptomatic treatment, including drinking fluids to prevent dehydration and administration of acetaminophen to relieve fever and pain.
Aspirin and other nonsteroidal anti-inflammatory drugs should be avoided until dengue infection has been ruled out, to reduce the risk of hemorrhage. Aspirin should not be used in children with acute viral illness because of its association with Reye syndrome.
The World Health Organization has issued initial guidance on psychosocial support for patients and families affected by Zika virus infection and associated complications.
There is currently no vaccine for Zika Virus but vaccine development is underway. Several inactivated vaccine candidates have been found to induce detectable neutralizing antibodies in phase I trials.
Prevention
Mosquito protection
Individuals in areas with risk for transmission should take measures to avoid mosquito bites, including personal protection as well as environmental control measures. Aedes mosquitoes bite during the daytime as well as at twilight; they breed in standing water (particularly manmade containers). Preventing mosquito bites by wearing long sleeves and long pants, using insect repellent, and staying indoors as feasible (with air conditioning, window/door screens, and/or mosquito nets to minimize contact between mosquitoes and people).
Individuals with Zika virus infection may reduce the spread of infection to others by following the same precautions to avoid mosquito bites during the first week of illness (the likely window of viremia).
Asymptomatic individuals who have traveled to an area with Zika virus mosquito transmission and then return to an area with no Zika virus mosquito transmission should avoid mosquito bites for three weeks after return (the period during which they could become viremic).
For people who have traveled to or live in areas of Zika virus mosquito transmission, it is important for individuals to abstain from sexual activity or use protection while active transmission persists. The World Health Organization (WHO), suggests that men and women outside areas of Zika transmission who have traveled to areas with active transmission wait at least six months following their return before unprotected sex, regardless of symptoms.
References
- Petersen LR, Jamieson DJ, Powers AM, Honein MA. Zika Virus. N Engl J Med 2016; 374:1552.
- Musso, D., & Gubler, D. J. (2016). Zika Virus. Clinical microbiology reviews, 29(3), 487–524. https://doi.org/10.1128/CMR.00072-15
- World Health Organization. Zika situation report. http://www.who.int/emergencies/zika-virus/situation-report/7-april-2016/en/ (Accessed on April 18, 2016).
- Musso, D., Nhan, T., Robin, E., Roche, C., Bierlaire, D., Zisou, K., Shan Yan, A., Cao-Lormeau, V. M., & Broult, J. (2014). Potential for Zika virus transmission through blood transfusion demonstrated during an outbreak in French Polynesia, November 2013 to February 2014. Euro surveillance : bulletin Europeen sur les maladies transmissibles = European communicable disease bulletin, 19(14), 20761. https://doi.org/10.2807/1560-7917.es2014.19.14.20761
- Dasgupta, S., Reagan-Steiner, S., Goodenough, D., Russell, K., Tanner, M., Lewis, L., Petersen, E. E., Powers, A. M., Kniss, K., Meaney-Delman, D., Oduyebo, T., O’Leary, D., Chiu, S., Talley, P., Hennessey, M., Hills, S., Cohn, A., Gregory, C., & Zika Virus Response Epidemiology and Laboratory Team (2016). Patterns in Zika Virus Testing and Infection, by Report of Symptoms and Pregnancy Status – United States, January 3-March 5, 2016. MMWR. Morbidity and mortality weekly report, 65(15), 395–399.
- Karwowski, M. P., Nelson, J. M., Staples, J. E., Fischer, M., Fleming-Dutra, K. E., Villanueva, J., Powers, A. M., Mead, P., Honein, M. A., Moore, C. A., & Rasmussen, S. A. (2016). Zika Virus Disease: A CDC Update for Pediatric Health Care Providers. Pediatrics, 137(5), e20160621.
- Sharp, T. M., Fischer, M., Muñoz-Jordán, J. L., Paz-Bailey, G., Staples, J. E., Gregory, C. J., & Waterman, S. H. (2019). Dengue and Zika Virus Diagnostic Testing for Patients with a Clinically Compatible Illness and Risk for Infection with Both Viruses. MMWR. Recommendations and reports : Morbidity and mortality weekly report. Recommendations and reports, 68(1), 1–10.
- Centers for Disease Control and Prevention. Zika Virus: Symptoms, Diagnosis, & Treatment. http://www.cdc.gov/zika/symptoms/index.html (Accessed on January 13, 2016).
- Brasil P, Vasconcelos Z, Kerin T, et al. Zika virus vertical transmission in children with confirmed antenatal exposure. Nat Commun 2020; 11:3510.